Risk Factors for Inpatient Hypoglycemia in a Tertiary Care Hospital in Indonesia
DOI:
https://doi.org/10.15605/jafes.037.02.06Keywords:
Hypoglycemia, diabetes, insulin, sulfonylurea, mortality, length of stay.Abstract
Introduction. Hypoglycemia is an important and harmful complication that often occurs in inpatient and outpatient settings. This study aims to assess the incidence of inpatient hypoglycemia and its related factors. We also assessed mortality and length of hospital stay.
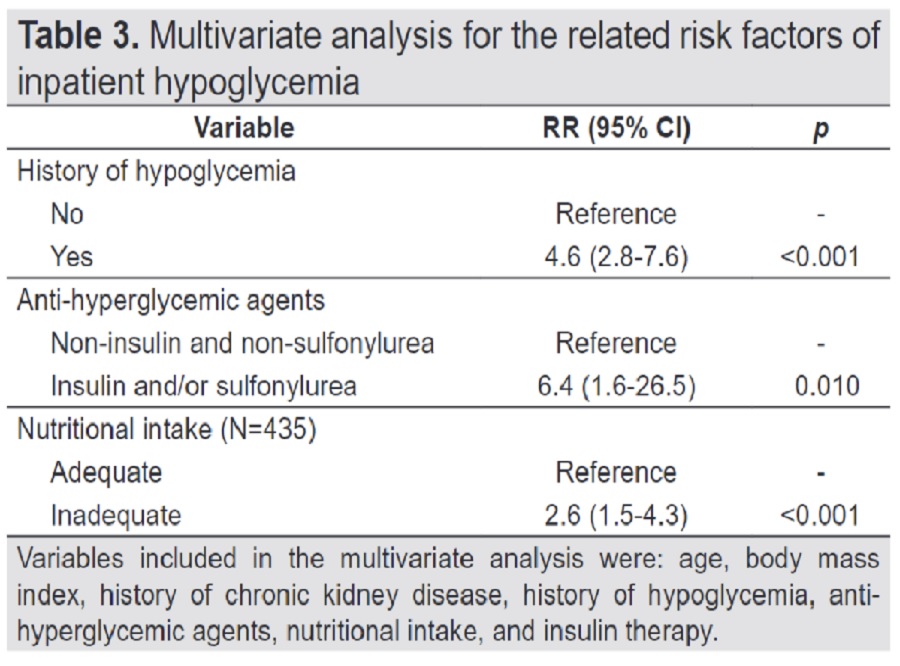
Methodology. We performed a retrospective cohort study among patients with type 2 diabetes mellitus admitted to a tertiary hospital in Indonesia. Using multivariate regression, we analyzed age, sex, body mass index, comorbidities, history of hypoglycemia, hyperglycemia treatment administered, nutritional intake, and medical instruction as the related risk factors for inpatient hypoglycemia.
Results. From 475 subjects, 80 (16.8%) had inpatient hypoglycemia, of which, 7.4% experienced severe hypoglycemia. We found that patients with a history of hypoglycemia (RR: 4.6; 95% CI: 2.8-7.6), insulin and/or sulfonylurea treatment (RR 6.4; 95% CI: 1.6-26.5), and inadequate nutritional intake (RR 2.6; 95% CI: 1.5-4.3) were more likely to have hypoglycemic events compared to those who did not. The length of hospital stay for patients in the hypoglycemic group is significantly longer than those in the non-hypoglycemic group (13 vs 7 days, p<0.001), but their mortality rates did not differ (16% vs 10.9%, p=0.18).
Conclusion. Inpatient hypoglycemia may be affected by a history of hypoglycemia and inadequate nutritional intake. Patients who had inpatient hypoglycemia tend to have a longer median length of hospital stay.
Downloads
References
Carey M, Boucai L, Zonszein J. Impact of hypoglycemia in hospitalized patients. Curr Diab Rep, 2013;13(1):107–13. https://pubmed.ncbi.nlm.nih.gov/23065370. https://doi.org/10.1007/s11892-012-0336-x.
Gómez-Huelgas R, Guijarro-Merino R, Zapatero A, et al. The frequency and impact of hypoglycemia among hospitalized patients with diabetes: A population-based study. J Diabetes Complications. 2015;29(8):1050-5. https://pubmed.ncbi.nlm.nih.gov/26279321. https://doi.org/10.1016/j.jdiacomp.2015.07.018.
UK Health and Social Care Information Centre. National Diabetes Inpatient Audit (NaDIA) - 2012. NHS Digital. UK: Healthcare Quality Improvement Partnership; 2013. Available from https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-inpatient-audit/national-diabetes-inpatient-audit-nadia-2012.
Rubin DJ, Golden SH. Hypoglycemia in non-critically ill, hospitalized patients with diabetes: Evaluation, prevention, and management. Hosp Pract (1995);2013;41(1):109-16. https://pubmed.ncbi.nlm.nih.gov/23466973. https://doi.org/10.3810/hp.2013.02.1016.
Maynard GA, Huynh MP, Renvall M. Iatrogenic inpatient hypoglycemia: Risk factors, treatment, and prevention. Diabetes Spectr. 2008;21(4):241–7.
Samaan NA. Hypoglycemia secondary to endocrine deficiencies. Endocrinol Metab Clin North Am. 1989;18(1):145–54. https://pubmed.ncbi.nlm.nih.gov/2537192.
Curkendall SM, Natoli JL, Alexander CM, Nathanson BH, Haidar T, Dubois RW. Economic and clinical impact of inpatient diabetic hypoglycemia Endocr Pr. 2009;15(4):302–12. https://pubmed.ncbi.nlm.nih.gov/19502209. https://doi.org/10.4158/EP08343.OR.
American Diabetes Association. 15. Diabetes care in the hospital: Standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Suppl 1):S211–20. https://pubmed.ncbi.nlm.nih.gov/33298426. https://doi.org/10.2337/dc21-S015.
Levin A, Stevens PE. Summary of KDIGO 2012 CKD guideline: Behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85(1):49–61. https://pubmed.ncbi.nlm.nih.gov/24284513. https://doi.org/10.1038/ki.2013.444.
Rattray M, Desbrow B, Roberts S. Comparing nutritional requirements, provision and intakes among patients prescribed therapeutic diets in hospital: An observational study. Nutrition. 2017;39–40:50–6. https://pubmed.ncbi.nlm.nih.gov/28606570. https://doi.org/10.1016/j.nut.2017.03.006.
American Diabetes Association. 12. Older adults: Standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Suppl 1):S168–79. https://pubmed.ncbi.nlm.nih.gov/33298423. https://doi.org/10.2337/dc21-S012.
LeRoith D, Biessels GJ, Braithwaite SS, et al. Treatment of diabetes in older adults: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2019;104(5):1520–74. https://pubmed.ncbi.nlm.nih.gov/30903688. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7271968. https://doi.org/10.1210/jc.2019-00198.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63. https://pubmed.ncbi.nlm.nih.gov/14726171. https://doi.org/10.1016/S0140-6736(03)15268-3.
Malone HE, Nicholl H, Coyne I. Fundamentals of estimating sample size. Nurse Res. 2016;23(5):21–5. https://pubmed.ncbi.nlm.nih.gov/27188569. https://doi.org/10.7748/nr.23.5.21.s5.
Akirov A, Amitai O, Masri-Iraqi H, et al. Predictors of hypoglycemia in hospitalized patients with diabetes mellitus. Intern Emerg Med. 2018;13(3):343–50. https://pubmed.ncbi.nlm.nih.gov/29340912. https://doi.org/10.1007/s11739-018-1787-0.
IBM Corp. IBM SPSS Statistics for Windows. Armonk, version 20.0. NY: IBM Corp; 2011.
Staley JR, Jones E, Kaptoge S, et al. A comparison of Cox and logistic regression for use in genome-wide association studies of cohort and case-cohort design. Eur J Hum Genet. 2017;25(7):854–62. https://pubmed.ncbi.nlm.nih.gov/28594416. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5520083. https://doi.org/10.1038/ejhg.2017.78.
Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression, 3rd ed. John Wiley & Sons, Inc.; 2013. Available from: https://doi.org/10.1002/9781118548387.refs.
Wexler DJ, Meigs JB, Cagliero E, Nathan DM, Grant RW. Prevalence of hyper- and hypoglycemia among inpatients with diabetes. Diabetes Care. 2007;30(2):367–9. https://pubmed.ncbi.nlm.nih.gov/17259511. https://doi.org/10.2337/dc06-1715.
American Diabetes Association. 6. Glycemic targets: Standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Suppl 1):S55–S64. https://pubmed.ncbi.nlm.nih.gov/29222377. https://doi.org/10.2337/dc18-S006.
Quilliam BJ, Simeone JC, Ozbay AB. Risk factors for hypoglycemia-related hospitalization in patients with type 2 diabetes : A nested case-control study. Clin Ther. 2011;33(11):1781–91. https://pubmed.ncbi.nlm.nih.gov/22018449. https://doi.org/10.1016/j.clinthera.2011.09.020.
Martín-Timón I, Del Cañizo-Gómez FJ. Mechanisms of hypoglycemia unawareness and implications in diabetic patients. World J Diabetes. 2015;6(7):912. https://pubmed.ncbi.nlm.nih.gov/26185599. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4499525. https://doi.org/10.4239/wjd.v6.i7.912.
Borzì V, Frasson G, Gussoni G, et al. Risk factors for hypoglycemia in patients with type 2 diabetes, hospitalized in internal medicine wards: Findings from the FADOI-DIAMOND study. Diabetes Res Clin Prac. 2016;115:24-30. https://pubmed.ncbi.nlm.nih.gov/27242119. https://doi.org/10.1016/j.diabres.2016.01.020.
Ignaczak A, Szymańska-Garbacz E, Kwiecińska E, Czupryniak L Risk factors for hypoglycaemia in in-patients with diabetes treated with continuous insulin intravenous infusion. Clin Diabetol. 2017;6(2):41-7. 10.5603/DK.2017.0008.
Holstein A, Plaschke A, Egberts EH. Lower incidence of severe hypoglycaemia in patients with type 2 diabetes treated with glimepiride versus glibenclamide. Diabetes Metab Res Rev. 2001;17(6):467–73. https://pubmed.ncbi.nlm.nih.gov/11757083. https://doi.org/10.1002/dmrr.235.
van Dalem J, Brouwers MCGJ, Stehouwer CDA, et al. Risk of hypoglycaemia in users of sulphonylureas compared with metformin in relation to renal function and sulphonylurea metabolite group: Population-based cohort study. BMJ. 2016;354:i3625. https://pubmed.ncbi.nlm.nih.gov/27413017. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4948031. https://doi.org/10.1136/bmj.i3625.
Schloot NC, Haupt A, Schütt M, et al. Risk of severe hypoglycemia in sulfonylurea-treated patients from diabetes centers in Germany/Austria: How big is the problem? Which patients are at risk? Diabetes Metab Res Rev. 2016;32(3):316–24. https://pubmed.ncbi.nlm.nih.gov/26409039. https://doi.org/10.1002/dmrr.2722.
Chew BH, Shariff Ghazali S, Ismail M, Haniff J, Bujang MA. Age ≥60years was an independent risk factor for diabetes-related complications despite good control of cardiovascular risk factors in patients with type 2 diabetes mellitus. Exp Gerontol. 2013;48(5):485–91. https://pubmed.ncbi.nlm.nih.gov/23454736. https://doi.org/10.1016/j.exger.2013.02.017.
National Health Ministry of Indonesia. Buku Kesehatan Lanjut Usia. Jakarta: National Health Ministry of Indonesia; 2016. Available from http://gizikia.kemkes.go.id/assets/file/pedoman/BUKU%20LANJUT%20USIA%20-%20Indonesia.pdf.
Chen WC, Lee CC, Chien MN, Liu SC, Wang CH, Yang WS. Blood glucose management of type 2 diabetes in the older people. Int J Gerontol. 2018;12(3):170-4. https://doi.org/10.1016/j.ijge.2018.05.008.
Freeman J. Management of hypoglycemia in older adults with type 2 diabetes. Postgrad Med. 2019;131(4):241–50. https://doi.org/10.1080/00325481.2019.1578590.
Gianchandani RY, Neupane S, Heung M. Hypoglycemia in hospitalized hemodialysis patients with diabetes: An observational study. J Diabetes Sci Technol. 2018;12(1):33–8. https://pubmed.ncbi.nlm.nih.gov/29291650. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5761994. https://doi.org/10.1177/1932296817747620.
Hsu PF, Sung SH, Cheng HM, et al. Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in type 2 diabetes: A nationwide population-based study. Diabetes Care. 2013;36(4):894–900. https://pubmed.ncbi.nlm.nih.gov/23223349. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3609481. https://doi.org/10.2337/dc12-0916.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Chici Pratiwi, Martin Rumende, Ida Ayu Made Kshanti , Pradana Soewondo

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Journal of the ASEAN Federation of Endocrine Societies is licensed under a Creative Commons Attribution-NonCommercial 4.0 International. (full license at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.
















