Prevalence of Diabetes Among Community-Living Older Persons in the Philippines:
The FITforFrail Study
DOI:
https://doi.org/10.15605/jafes.037.02.15Keywords:
diabetes, older persons, comorbiditiesAbstract
Objective. To estimate the prevalence of diabetes among Filipino older persons living in the community.
Methodology. A cross-sectional analysis was done on a random sample of persons ages 60 years and older from the Focused Interventions for Frail Older Adults Research and Development Program (2018-2019). A diagnosis of diabetes was established by self-reported physician’s diagnosis or if the person was on any antihyperglycemic drugs.
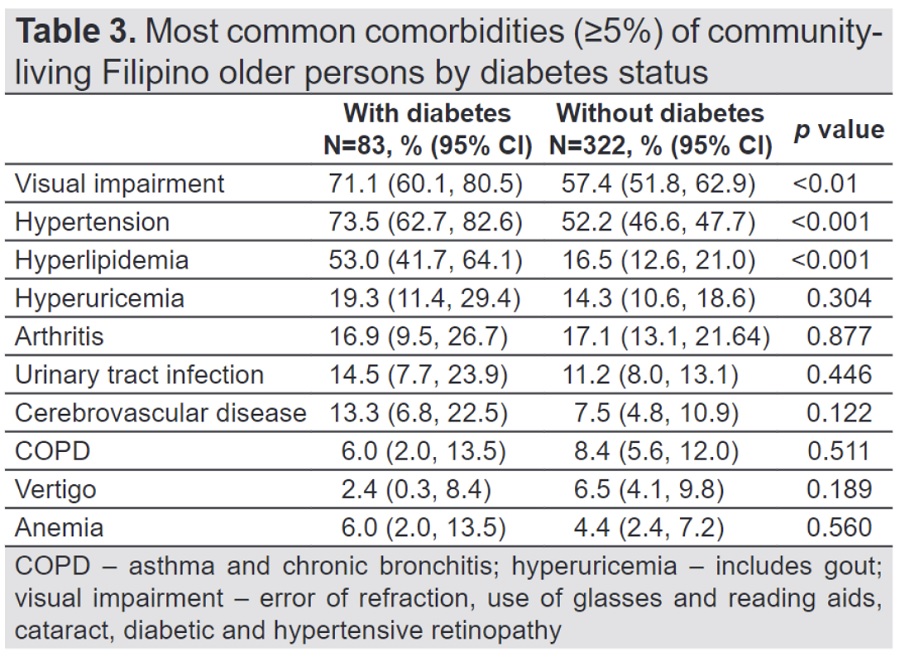
Results. The prevalence of self-reported diabetes was 20.5%, with no difference in age, sex, education, or body mass index between older persons with and without diabetes. The presence of 2 or more comorbidities was significantly more common among older persons with diabetes (p<0.001). Visual impairment (p<0.01), hypertension (p<0.001) and hyperlipidemia (p <0.001) were more frequent among those with diabetes.
Conclusion. Diabetes is prevalent among community-living older Filipinos. Therefore, effective public health measures for diabetes prevention and management are needed for the ever-growing older population, who are at the highest risk for morbidity and mortality.
Downloads
References
International Diabetes Federation. Diabetes Estimates (20-79). IDF Diabetes Atlas 10th ed.; 2021. Available from https://diabetesatlas.org/data/en/indicators/1/. Accessed 29 March 2022.
Sinclair A, Saeedi P, Kaundal A, Karuranga S, Malanda B, Williams R. Diabetes and global ageing among 65-99-year-old adults: Findings from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2020;162:108078. https://pubmed.ncbi.nlm.nih.gov/32068097. https://doi.org/10.1016/j.diabres.2020.108078.
World Health Organization. Global Health Estimates: Life expectancy and leading causes of death and disability. Available from https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death. Accessed 30 March 2022.
van Dieren S, Beulens JW, van der Schouw YT, Grobbee DE, Neal B. The global burden of diabetes and its complications: An emerging pandemic. Eur J Cardiovasc Prev Rehabil. 2010;17 Suppl 1:S3-8. https://pubmed.ncbi.nlm.nih.gov/20489418. https://doi.org/10.1097/01.hjr.0000368191.86614.5a.
Forbes A, Murrells T, Sinclair AJ. Examining factors associated with excess mortality in older people (age ≥70 years) with diabetes - A 10-year cohort study of older people with and without diabetes. Diabet Med.2017;34(3):387–95. https://pubmed.ncbi.nlm.nih.gov/27087619. https://doi.org/10.1111/dme.13132.
Saeedi P, Salpea P, Karuranga S, et al. Mortality attributable to diabetes in 20-79 years old adults, 2019 estimates: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2020;162:108086.https://pubmed.ncbi.nlm.nih.gov/32068099. https://doi.org/10.1016/j.diabres.2020.108086.
Tzoulaki, I, Molokhia, M, Curcin, V, et al. Risk of cardiovascular disease and all-cause mortality among patients with type 2 diabetes prescribed oral antidiabetic drugs: Retrospective cohort study using UK general practice research database. BMJ. 2009;339:b4731. https://pubmed.ncbi.nlm.nih.gov/19959591. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2788912. https://doi.org/10.1136/bmj.b4731.
World Health Organization. Multimorbidity. Geneva: World Health Organization; 2016. Available from https://apps.who.int/iris/bitstream/handle/10665/252275/9789241511650-eng.pdf. Accessed 25 March 2022.
Guerrero-Fernández de Alba I, Orlando V, Monetti VM, et al. Comorbidity in an older population with type 2 diabetes mellitus: Identification of the characteristics and healthcare utilization of high-cost patients. Front Pharmacol. 2020;11:586187. https://pubmed.ncbi.nlm.nih.gov/33746740. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7970761. https://doi.org/10.3389/fphar.2020.586187.
Gruneir A, Markle-Reid M, Fisher K, Reimer H, Ma X, Ploeg J. Comorbidity burden and health services use in community-living older adults with diabetes mellitus: A retrospective cohort study. Can J Diabetes. 2016;40(1):35-42. https://pubmed.ncbi.nlm.nih.gov/26778680. https://doi.org/10.1016/j.jcjd.2015.09.002.
Fisher K, Griffith L, Gruneir A, et al. Comorbidity and its relationship with health service use and cost in community-living older adults with diabetes: A population-based study in Ontario, Canada. Diabetes Res Clin Pract. 2016;122:113-23. https://pubmed.ncbi.nlm.nih.gov/27833049. https://doi.org/10.1016/j.diabres.2016.10.009.
Halter JB, Musi N, McFarland Horne F, et al. Diabetes and cardiovascular disease in older adults: Current status and future directions. Diabetes. 2014;63(8):2578–89. https://pubmed.ncbi.nlm.nih.gov/25060886. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4113072. https://doi.org/10.2337/db14-0020.
Kirkman MS, Briscoe VJ, Clark N, et al. Consensus development conference on diabetes and older adults. Diabetes in older adults: A consensus report. J Am Geriatr Soc. 2012;60(12):2342–56. https://pubmed.ncbi.nlm.nih.gov/23106132. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4525769. https://doi.org/10.1111/jgs.12035.
Kalyani RR, Saudek CD, Brancati FL, Selvin E. Association of diabetes, comorbidities, and A1C with functional disability in older adults: Results from the National Health and Nutrition Examination Survey (NHANES), 1999-2006. Diabetes Care. 2010;33(5):1055-60. https://pubmed.ncbi.nlm.nih.gov/20185736. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2858174. https://doi.org/10.2337/dc09-1597.
Volpato S, Maraldi C, Fellin R. Type 2 diabetes and risk for functional decline and disability in older persons. Curr Diabetes Rev. 2010;6(3):134-43. https://pubmed.ncbi.nlm.nih.gov/20380626. https://doi.org/10.2174/157339910791162961.
Department of Economics and Social Affairs. Population Dynamics. United Nations. Available from https://population.un.org/wpp/DataQuery/. Accessed 29 March 2022.
Philippine Statistics Authority. Causes of death in the Philippines (preliminary): January to December 2021. Available from https://psa.gov.ph/content/causes-deaths-philippines-preliminary-january-december-2021. Accessed 30 March 2022.
Philippine Council for Health Research and Development. FITforFrail Final Report. Study 2. Mixed method studies on health status of older adults with focus on frailty among older persons in select communities.
NIH Geriatric assessment methods for clinical decision making. NIH Consensus Statement Online 1987 Oct Online 19-21;6(13):1-21. Available from https://consensus.nih.gov/1987/1987geriatricassessment065html.htm. Accessed 20 March 2022.
World Health Organization. The Asia Pacific perspective: Redefining obesity and its treatment. WHO Western Pacific Region; 2000. Available from https://apps.who.int/iris/bitstream/handle/10665/206936/0957708211_eng.pdf?sequence=1&isAllowed=y. Accessed 28 March 2022.
Salas A, Acosta D, Ferri CP, et al. The prevalence, correlates, detection and control of diabetes among older people in low and middle income countries. A 10/66 Dementia Research Group Population-Based Survey. PLoS One. 2016;11(2):e0149616. https://pubmed.ncbi.nlm.nih.gov/26913752. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4767439. https://doi.org/10.1371/journal.pone.0149616.
Brown AF, Ettner SL, Piette J, et al. Socioeconomic position and health among persons with diabetes mellitus: A conceptual framework and review of the literature. Epidemiol Rev. 2004;26:63-77. https://pubmed.ncbi.nlm.nih.gov/15234948. https://doi.org/10.1093/epirev/mxh002.
Ho BK, Jasvindar K, Gurpreet K, et al. Prevalence, awareness, treatment and control of diabetes mellitus among the elderly: The 2011 National Health and Morbidity Survey, Malaysia. Malays Fam Physician. 2014;9(3):12-9. https://pubmed.ncbi.nlm.nih.gov/26425300. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4568721.
Tanoey J, Becher H. Diabetes prevalence and risk factors of early-onset adult diabetes: Results from the Indonesian family life survey. Glob Health Action. 2021;14(1):2001144. https://pubmed.ncbi.nlm.nih.gov/34898388. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8676618. https://doi.org/10.1080/16549716.2021.2001144.
Garcia A, De la Vega S, Giron MST, Fabito SJ. The visual and hearing impairments among working and retired employees with type 2 diabetes mellitus in two academic communities in the Philippines. Acta Medica Philipp. 2022;56(3):72-81. https://doi.org/10.47895/amp.vi0.3133
Rockwood K, Tan M, Phillips S, McDowell I. Prevalence of diabetes mellitus in elderly people in Canada: Report from the Canadian Study of Health and Aging. Age Ageing. 1998;27(5):573-7. https://pubmed.ncbi.nlm.nih.gov/12675096. https://doi.org/10.1093/ageing/27.5.573.
Shang Y, Marseglia A, Fratiglioni L, et al. Natural history of prediabetes in older adults from a population-based longitudinal study. J Intern Med. 2019;286(3):326-340. https://pubmed.ncbi.nlm.nih.gov/31165572. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6851857. https://doi.org/10.1111/joim.12920.
Chiang JI, Hanlon P, Li TC, et al. Multimorbidity, mortality, and HbA1c in type 2 diabetes: A cohort study with UK and Taiwanese cohorts. PLoS Med. 2020;17(5):e1003094. https://pubmed.ncbi.nlm.nih.gov/32379755. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7205223. https://doi.org/10.1371/journal.pmed.1003094.
Du Y, Heidemann C, Gößwald A, Schmich P, Scheidt-Nave C. Prevalence and comorbidity of diabetes mellitus among non-institutionalized older adults in Germany - Results of the national telephone health interview survey 'German Health Update (GEDA)' 2009. BMC Public Health. 2013;13:166. https://pubmed.ncbi.nlm.nih.gov/23433228. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3599814. https://doi.org/10.1186/1471-2458-13-166.
Huang ES. Management of diabetes mellitus in older people with comorbidities. BMJ. 2016;353:i2200. https://pubmed.ncbi.nlm.nih.gov/27307175. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6884153. https://doi.org/10.1136/bmj.i2200.
Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29(3):725-31. https://pubmed.ncbi.nlm.nih.gov/16505540. https://doi.org/10.2337/diacare.29.03.06.dc05-2078.
Bo M, Gallo S, Zanocchi M, et al. Prevalence, clinical correlates, and use of glucose-lowering drugs among older patients with type 2 diabetes living in long-term care facilities. J Diabetes Res. 2015;2015:174316. https://pubmed.ncbi.nlm.nih.gov/26425567. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4575744. https://doi.org/10.1155/2015/174316.
Sánchez Martínez M, Blanco A, Castell MV, et al. Diabetes in older people: Prevalence, incidence and its association with medium- and long-term mortality from all causes. Aten Primaria. 2014;46(7):376-84. https://pubmed.ncbi.nlm.nih.gov/24576691. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6983613. https://doi.org/10.1016/j.aprim.2013.12.004.
Junker K, Buckley CM, Millar SR, et al. The prevalence and correlates of pre-diabetes in middle- to older-aged Irish adults using three diagnostic methods. PLoS One. 2021;16(6):e0253537. https://pubmed.ncbi.nlm.nih.gov/34170932. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8232457. https://doi.org/10.1371/journal.pone.0253537.
Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: A systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):804-18. https://pubmed.ncbi.nlm.nih.gov/21335614. https://doi.org/10.1093/ije/dyr029.
Reed J, Bain S, Kanamarlapudi V. A review of current trends with type 2 diabetes epidemiology, aetiology, pathogenesis, treatments and future perspectives. Diabetes Metab Syndr Obes. 2021;14:3567-3602. https://pubmed.ncbi.nlm.nih.gov/34413662. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8369920. https://doi.org/10.2147/DMSO.S319895.
Golay A, Ybarra J. Link between obesity and type 2 diabetes. Best Pract Res Clin Endocrinol Metab. 2005;19(4):649–63. https://pubmed.ncbi.nlm.nih.gov/16311223. https://doi.org/10.1016/j.beem.2005.07.010
Kashima S, Inoue K, Matsumoto M, Akimoto K. Prevalence and characteristics of non-obese diabetes in Japanese men and women: The Yuport Medical Checkup Center Study. J Diabetes. 2015;7(4):523-30. https://pubmed.ncbi.nlm.nih.gov/25196076. https://doi.org/10.1111/1753-0407.12213.
Nakagami T, Qiao Q, Carstensen B, et al. Age, body mass index and type 2 diabetes-associations modified by ethnicity. Diabetologia. 2003;46(8):1063-70. https://pubmed.ncbi.nlm.nih.gov/12827246. https://doi.org/10.1007/s00125-003-1158-9.
Bush TL, Miller SR, Golden AL, Hale WE. Self-report and medical record report agreement of selected medical conditions in the elderly. Am J Public Health. 1989;79(11):1554-6. https://pubmed.ncbi.nlm.nih.gov/2817172. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1349815. https://doi.org/10.2105/ajph.79.11.1554.
Comino EJ, Tran DT, Haas M, et al. Validating self-report of diabetes use by participants in the 45 and Up Study: A record linkage study. BMC Health Serv Res. 2013;13:481. https://pubmed.ncbi.nlm.nih.gov/24245780. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3893423. https://doi.org/10.1186/1472-6963-13-481.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Maria Stella Giron, Shelley Ann de la Vega

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Journal of the ASEAN Federation of Endocrine Societies is licensed under a Creative Commons Attribution-NonCommercial 4.0 International. (full license at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.
















