Incidence, Recurrence and Mortality among Filipinos with Differentiated Thyroid Cancer
A Systematic Review
DOI:
https://doi.org/10.15605/jafes.038.01.14Keywords:
Filipino, thyroid malignancy, differentiated thyroid carcinoma, papillary thyroid carcinoma, follicular thyroid carcinomaAbstract
Background. The majority of thyroid malignancies are differentiated thyroid carcinomas (DTCs). We examined the incidence, disease extent, recurrence and disease-specific mortality (DSM) of DTC among Filipinos residing in the Philippines and Filipino immigrants.
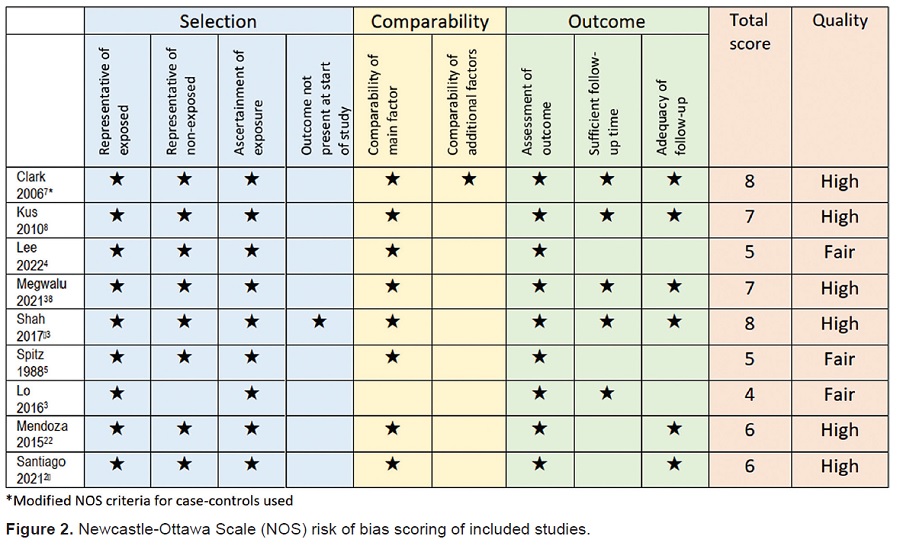
Methodology. In accordance with the 2020 PRISMA statement, we performed a systematic literature search in MEDLINE, Google Scholar, EBSCO, Cochrane and Clinicaltrials.gov for the period January 1, 1980 until January 27, 2022. Pooled incidence rate ratio and pooled proportions of disease extent, recurrence and DSM were determined.
Results. Literature search yielded 1,852 studies. Out of 26 articles retrieved, nine retrospective case controls and cohorts were included. Incidence of DTC was significantly higher in female Filipino immigrants compared with non-Hispanic whites (NHW). Distant metastases and recurrence were more common among Filipinos and Filipino immigrants compared with NHW. Limited data showed higher DSM in Filipino immigrants and NHW than Filipinos, which may be influenced by reporting bias.
Conclusions. This review supports the trend of increased incidence and recurrence of DTC among Filipinos, although case registries are essential to confirm these findings. In the setting of the newly released Philippine guidelines for DTC, prospective studies with active long-term follow-up will help detect any changes in the outcomes of DTC among Filipinos.
Downloads
References
Tiangco B, Nuique R, Flores J. 2020 Cancer Registry and Research Annual Report. 2020. https://careph.org/wp-content/uploads/2021/04/2020-ANNUAL-REPORT_Final-final.pdf.
Filetti SR, Tuttle, Michael Leboulleux S, Alexander EK. Nontoxic diffuse goiter, nodular thyroid disorders, and thyroid malignancies. In: Williams Textbook of Endocrinology;2020.
Lo TEN, Uy AT, Maningat PDD. Well-differentiated thyroid cancer: The Philippine General Hospital experience. Endocrinol Metab (Seoul). 2016;31(1):72–9. https://pubmed.ncbi.nlm.nih.gov/26754584. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4803565. https://doi.org/10.3803/EnM.2016.31.1.72.
Lee AW, Mendoza RA, Aman S, Hsu R, Liu L. Thyroid cancer incidence disparities among ethnic Asian American populations, 1990–2014. Ann Epidemiol. 2022;66:28–36. https://pubmed.ncbi.nlm.nih.gov/34774744. https://doi.org/10.1016/j.annepidem.2021.11.002.
Spitz MR, Katz RL, Pollack ESPOL, Newell GR. Ethnic patterns of thyroid cancer incidence in the United States, 1973-1981. Int J Cancer. 1988;42(4):549–53. https://pubmed.ncbi.nlm.nih.gov/3170027. https://doi.org/10.1002/ijc.2910420413.
Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. https://pubmed.ncbi.nlm.nih.gov/26462967. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4739132. https://doi.org/10.1089/thy.2015.0020.
Clark JR, Eski SJ, Freeman JL. Risk of malignancy in Filipinos with thyroid nodules—A matched pair analysis. Head Neck. 2006;28(5):427–31.
Kus LH, Shah M, Eski S, Walfish PG, Freeman JL. Thyroid cancer outcomes in Filipino patients. Arch Otolaryngol - Head Neck Surg. 2010;136(2):138–42. https://pubmed.ncbi.nlm.nih.gov/16287137. https://doi.org/10.1002/hed.20333.
Department of Health. The Philippine Interim Clinical Practice Guidelines for the Diagnosis and Management of Well-Differentiated Thyroid Cancer 2021. Philippine College of Surgeons. 2021. https://pcs.org.ph/wp-content/uploads/2022/03/finalThyroid-CA-CPG_manuscript_220220-5.pdf.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://pubmed.ncbi.nlm.nih.gov/33782057. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8005924. https://doi.org/10.1136/bmj.n71.
Carlos-Raboca J, Jimeno CA, Kho SA, et al. The Philippine Thyroid Diseases Study (PhilTiDeS 1): Prevalence of thyroid disorders among adults in the Philippines. J ASEAN Fed Endocr Soc. 2014;27(1):27–33. https://doi.org/10.15605/jafes.027.01.05.
Laudico A, Mirasol-Lumague MR, Medina V, Mapua C, Valenzuela FG, Pukkala E. 2015 Philippine cancer facts and estimates. Manila; 2015. http://thepafp.org/website/wp-content/uploads/2017/05/2015-PCS-Ca-Facts-Estimates_CAN090516.pdf.
Shah BR, Griffiths R, Hall SF. Thyroid cancer incidence among Asian immigrants to Ontario, Canada: A population-based cohort study. Cancer. 2017;123(17):3320–5. https://pubmed.ncbi.nlm.nih.gov/28440952. https://doi.org/10.1002/cncr.30746.
Megwalu UC, Osazuwa‐Peters N, Moon P, Palaniappan LP. Thyroid cancer incidence trends among Filipinos in the United States. Laryngoscope. 2022;132(7):1495-1502. https://pubmed.ncbi.nlm.nih.gov/34910822. https://doi.org/10.1002/lary.29986.
Shobab L, Burman KD, Wartofsky L. Sex differences in differentiated thyroid cancer. Thyroid. 2021;32(3):224–35. https://pubmed.ncbi.nlm.nih.gov/34969307. https://doi.org/10.1089/thy.2021.0361.
Li P, Ding Y, Liu M, Wang W, Li X. Sex disparities in thyroid cancer: A SEER population study. Gland Surg. 2021;10(12):3200–10. https://pubmed.ncbi.nlm.nih.gov/35070880. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8749097. https://doi.org/10.21037/gs-21-545.
Horn-Ross PL, McClure LA, Chang ET, et al. Papillary thyroid cancer incidence rates vary significantly by birthplace in Asian American women. Cancer Causes Control. 2011;22(3):479–85. https://pubmed.ncbi.nlm.nih.gov/21207130. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3291661. https://doi.org/10.1007/s10552-010-9720-5.
Grebe SK, Hay ID. Thyroid cancer nodal metastases: Biologic significance and therapeutic considerations. Surg Oncol Clin N Am. 1996;5(1):43–63. https://pubmed.ncbi.nlm.nih.gov/8789493.
Asari R, Koperek O, Scheuba C, et al. Follicular thyroid carcinoma in an iodine-replete endemic goiter region. Ann Surg. 2009;249(6):1023–31. https://pubmed.ncbi.nlm.nih.gov/19474675. https://doi.org/10.1097/SLA.0b013e3181a77b7b.
Leboulleux S, Rubino C, Baudin E, et al. Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab. 2005;90(10):5723–9. https://pubmed.ncbi.nlm.nih.gov/16030160. https://doi.org/10.1210/jc.2005-0285.
Santiago AG, Isidro MJ, Parra J. Predictors of response to therapy among post thyroidectomy adult filipino patients with papillary thyroid carcinoma based on the 2015 American Thyroid Association Guidelines. J ASEAN Fed Endocr Soc. 2021;36(2):161–6. https://pubmed.ncbi.nlm.nih.gov/34966200. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8666484. https://doi.org/10.15605/jafes.036.02.18.
Mendoza ES, Lopez AA, Valdez VAU, et al. Predictors of incomplete response to therapy among Filipino patients with papillary thyroid cancer in a tertiary hospital. J Endocrinol Invest. 2016;39(1):55-62. https://pubmed.ncbi.nlm.nih.gov/26036600. https://doi.org/10.1007/s40618-015-0319-2.
Lo TE, Canto AU, Maningat PDD. Risk factors for recurrence in filipinos with well-differentiated thyroid cancer. Endocrinol Metab. 2015;30(4):543–50. https://pubmed.ncbi.nlm.nih.gov/26485470. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4722410. https://doi.org/10.3803/EnM.2015.30.4.543.
Nguyen MLT, Hu J, Hastings KG, et al. Thyroid cancer mortality is higher in Filipinos in the United States: An analysis using national mortality records from 2003 through 2012. Cancer. 2017;123(24):4860–7. https://pubmed.ncbi.nlm.nih.gov/28881423. Phttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC5716919. https://doi.org/10.1002/cncr.30958.
Vuong HG, Altibi AMA, Abdelhamid AH, et al. The changing characteristics and molecular profiles of papillary thyroid carcinoma over time: a systematic review. Oncotarget. 2017;8(6):10637–49. https://pubmed.ncbi.nlm.nih.gov/27793009. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5354688. https://doi.org/10.18632/oncotarget.12885.
Romei C, Elisei R. A Narrative review of genetic alterations in primary thyroid epithelial cancer. Int J Mol Sci. 2021;22(4):1726. https://pubmed.ncbi.nlm.nih.gov/33572167. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7915177. https://doi.org/10.3390/ijms22041726.
Navarro-Locsin CG, Chang AMV, Daroy ML, Alfon AC, Andal JJ, Padua PF. Clinical and histopathological profile of BRAF V600E mutation in conventional papillary thyroid carcinoma in a Filipino population. Malays J Pathol. 2016;38(2):141–8. https://pubmed.ncbi.nlm.nih.gov/27568671.
Espiritu GAM, Malana JT, Dumasis AJG V, Ang DC. High preponderance of BRAF V600E mutation in papillary thyroid carcinoma among Filipinos: A clinicopathologic study. J Glob Oncol. 2019;2019(5):1–6. https://pubmed.ncbi.nlm.nih.gov/30694737. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6426509. https://doi.org/10.1200/JGO.18.00085.
Morita SY, Grace CK, Lum CA, Davis JW. Abstract B76: Thyroid cancer ethnic disparity in Hawaii: BRAF mutation within the Filipino population. Cancer Epidemiol Biomarkers Prev. 2011;20(Suppl 10):B76. https://doi.org/10.1158/1055-9965.DISP-11-B76.
Mathur A, Moses W, Rahbari R, et al. Higher rate of BRAF mutation in papillary thyroid cancer over time. Cancer. 2011;117(19):4390–5. https://pubmed.ncbi.nlm.nih.gov/21412762. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3131457. https://doi.org/10.1002/cncr.26072.
Jung CK, Little MP, Lubin JH, , et al. The increase in thyroid cancer incidence during the last four decades is accompanied by a high frequency of BRAF mutations and a sharp increase in RAS mutations. J Clin Endocrinol Metab. 2014;99(2):E276–85. https://pubmed.ncbi.nlm.nih.gov/24248188. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3913801. https://doi.org/10.1210/jc.2013-2503.
Romei C, Fugazzola L, Puxeddu E, et al. Modifications in the papillary thyroid cancer gene profile over the last 15 years. J Clin Endocrinol Metab. 2012;97(9):E1758–65. https://pubmed.ncbi.nlm.nih.gov/22745248. https://doi.org/10.1210/jc.2012-1269.
Nam JK, Jung CK, Song BJ, et al. Is the BRAF(V600E) mutation useful as a predictor of preoperative risk in papillary thyroid cancer? Am J Surg. 2012;203(4):436–41. https://pubmed.ncbi.nlm.nih.gov/21803329. https://doi.org/10.1016/j.amjsurg.2011.02.013.
Rood K, Begum K, Wang H, et al. Differential expression of non-coding rna signatures in thyroid cancer between two ethnic groups. Curr Oncol. 2021;28(5):3610–28. https://pubmed.ncbi.nlm.nih.gov/34590612. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8482137. https://doi.org/10.3390/curroncol28050309.
Tuttle RM, Tala H, Shah J, et al. Estimating risk of recurrence in differentiated thyroid cancer after total thyroidectomy and radioactive iodine remnant ablation: Using response to therapy variables to modify the initial risk estimates predicted by the New American Thyroid Association. Thyroid. 2010;20(12):1341–9. https://pubmed.ncbi.nlm.nih.gov/21034228. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4845674. https://doi.org/10.1089/thy.2010.0178.
Vaisman F, Momesso D, Bulzico DA, et al. Spontaneous remission in thyroid cancer patients after biochemical incomplete response to initial therapy. Clin Endocrinol (Oxf). 2012;77(1):132–8. https://pubmed.ncbi.nlm.nih.gov/22248037. https://doi.org/10.1111/j.1365-2265.2012.04342.x.
Pitoia F, Bueno F, Urciuoli C, Abelleira E, Cross G, Tuttle RM. Outcomes of patients with differentiated thyroid cancer risk-stratified according to the American Thyroid Association and Latin American Thyroid Society risk of recurrence classification systems. Thyroid. 2013;23(11):1401–7. https://pubmed.ncbi.nlm.nih.gov/23517313. https://doi.org/10.1089/thy.2013.0011.
Megwalu UC, Ma Y, Osazuwa-Peters N, Orloff LA. Clinical presentation and survival outcomes of well-differentiated thyroid cancer in Filipinos. Cancer Med. 2021;10(17):5964–73. https://pubmed.ncbi.nlm.nih.gov/34288520. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8419748. https://doi.org/10.1002/cam4.4149.
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Mari Des San Juan, Elizabeth Paz-Pacheco

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Journal of the ASEAN Federation of Endocrine Societies is licensed under a Creative Commons Attribution-NonCommercial 4.0 International. (full license at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.
















