Adaptation and Validation of the Vietnamese-Translated Diabetes Knowledge Questionnaire
DOI:
https://doi.org/10.15605/jafes.037.01.08Keywords:
Diabetes, diabetes knowledge questionnaire, translation, VietnameseAbstract
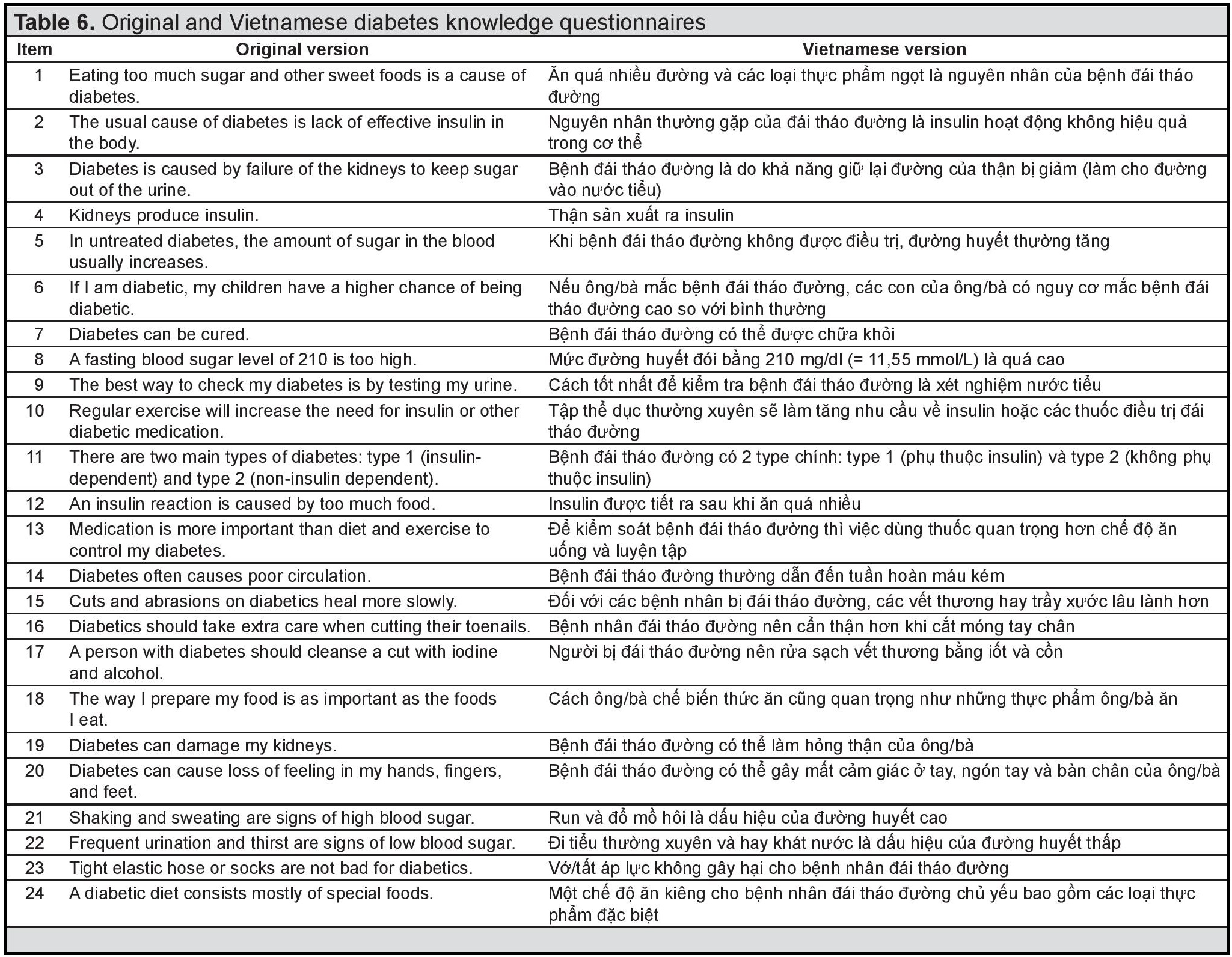
Objectives. There is no existing Vietnamese diabetes knowledge questionnaire. This impedes assessment of patient knowledge that will be helpful in providing effective diabetes intervention. We aimed to validate the Vietnamese-translated Diabetes Knowledge Questionnaire (DKQ).
Methodology. Translation and adaptation strictly followed the guidelines of Beaton et al. Internal consistency was assessed by Cronbach’s alpha coefficient, test-retest reliability was assessed by Fleiss’ Kappa coefficient, and validity value was determined among type 2 diabetes patients in a general hospital.
Results. The Vietnamese version of the DKQ had good internal consistency (Cronbach’s alpha for all items = 0.898) and stability (Kappa coefficient >0.600). The average score for all equivalence criteria was 1.00, demonstrating good equivalence to the original. The significant difference between knowledge score and education level (p <0.001) confirmed construct validity.
Conclusion. Our study provided a reliable Vietnamese version of the DKQ. Future studies may apply the version in different regions in Vietnam to determine external validity.
Downloads
References
Raaijmakers LGM, Martens MK, Bagchus C, de Weerdt I, de Vries NK, Kremers SPJ. Correlates of perceived self-care activities and diabetes control among Dutch type 1 and type 2 diabetics. J Behav Med. 2015;38(3):450-9. https://pubmed.ncbi.nlm.nih.gov/25627667. https://doi.org/10.1007/s10865-014-9609-y.
Rowley WR, Bezold C, Arikan Y, Byrne E, Krohe S. Diabetes 2030: Insights from yesterday, today, and future trends. Popul Health Manag. 2017;20(1):6-12. https://pubmed.ncbi.nlm.nih.gov/27124621. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5278808. https://doi.org/10.1089/pop.2015.0181.
Klonoff DC. The increasing incidence of diabetes in the 21st century. J Diabetes Sci Technol. 2009;3(1):1-2. https://pubmed.ncbi.nlm.nih.gov/20046646. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2769839. https://doi.org/10.1177%2F193229680900300101.
Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. https://pubmed.ncbi.nlm.nih.gov/31518657. https://doi.org/10.1016/j.diabres.2019.107843.
International Diabetes Federation. IDF Diabetes Atlas. 10th ed. Brussels, Belgium: International Diabetes Federation, 2021. https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf.
Ngoc NB, Lin ZL, Ahmed W. Diabetes: What challenges lie ahead for Vietnam? Ann Glob Health. 2020;86(1):1. https://pubmed.ncbi.nlm.nih.gov/31934549. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6952858. https://doi.org/10.5334/aogh.2526.
World Health Organization. The growing burden of diabetes in Viet Nam. https://www.who.int/vietnam/news/feature-stories/detail/the-growing-burden-of-diabetes-in-viet-nam. Accessed November 15, 2021.
Sweileh WM, Zyoud SH, Abu Nab'a RJ, et al. Influence of patients' disease knowledge and beliefs about medicines on medication adherence: Findings from a cross-sectional survey among patients with type 2 diabetes mellitus in Palestine. BMC Public Health. 2014;14:94. https://pubmed.ncbi.nlm.nih.gov/24479638. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3909379. https://doi.org/10.1186/1471-2458-14-94.
Lu M, Xia H, Ma J, et al. Relationship between adherence to secondary prevention and health literacy, self-efficacy and disease knowledge among patients with coronary artery disease in China. Eur J Cardiovasc Nurs. 2020;19:(3):230-7. https://pubmed.ncbi.nlm.nih.gov/31595771. https://doi.org/10.1177/1474515119880059.
Jiraporncharoen W, Pinyopornpanish K, Junjom K, et al. Exploring perceptions, attitudes and beliefs of Thai patients with type 2 diabetes mellitus as they relate to medication adherence at an out-patient primary care clinic in Chiang Mai, Thailand. BMC Fam Pract. 2020;21(1):173. https://pubmed.ncbi.nlm.nih.gov/32825811. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7442984. https://doi.org/10.1186/s12875-020-01233-7.
Khalesi S, Irwin C, Sun J. Dietary patterns, nutrition knowledge, lifestyle, and health-related quality of life: Associations with anti-hypertension medication adherence in a sample of Australian adults. High Blood Press Cardiovasc Prev. 2017;24(4):453-62. https://pubmed.ncbi.nlm.nih.gov/28884295. https://doi.org/10.1007/s40292-017-0229-9.
Almas A, Godil SS, Lalani S, Samani ZA, Khan AH. Good knowledge about hypertension is linked to better control of hypertension: A multicentre cross sectional study in Karachi, Pakistan. BMC Res Notes. 2012;5:579. https://pubmed.ncbi.nlm.nih.gov/23095492. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3534478. https://doi.org/10.1186/1756-0500-5-579.
Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99(6):926-43. https://pubmed.ncbi.nlm.nih.gov/26658704. https://doi.org/10.1016/j.pec.2015.11.003.
Gucciardi E, Chan VWS, Manuel L, Sidani S. A systematic literature review of diabetes self-management education features to improve diabetes education in women of Black African/Caribbean and Hispanic/Latin American ethnicity. Patient Educ Couns. 2013;92(2):235-45. https://pubmed.ncbi.nlm.nih.gov/23566428. https://doi.org/10.1016/j.pec.2013.03.007.
Pousinho S, Morgado M, Falcão A, Alves G. Pharmacist interventions in the management of type 2 diabetes mellitus: A systematic review of randomized controlled trials. J Manag Care Spec Pharm. 2016;22(5):493-515. https://pubmed.ncbi.nlm.nih.gov/27123912. https://doi.org/10.18553/jmcp.2016.22.5.493.
Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: A systematic review. Pharmacotherapy. 2008;28(4):421-36. https://pubmed.ncbi.nlm.nih.gov/18363526. https://doi.org/10.1592/phco.28.4.421.
Adibe MO, Aguwa CN, Ukwe CV. The construct validity of an instrument for measuring type 2 diabetes self-care knowledge in Nigeria. Trop J Pharm Res. 2011;10(5):619-29. https://doi.org/10.4314/tjpr.v10i5.11.
Fitzgerald JT, Funnell MM, Hess GE, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998;21(5):706-10. https://pubmed.ncbi.nlm.nih.gov/9589228. https://doi.org/10.2337/diacare.21.5.706.
UNESCO Institute for Statistics. Educational attainment, at least Bachelor’s or equivalent, population 25+, total (%) (cumulative). https://data.worldbank.org/indicator/SE.TER.CUAT.BA.ZS. Accessed November 15, 2021.
Quy N. Vietnam slips in English proficiency rankings. https://e.vnexpress.net/news/news/vietnam-slips-in-english-proficiency-rankings-4192970.html.
Garcia AA, Villagomez ET, Brown SA, Kouzekanani K, Hanis CL. The Starr County Diabetes Education Study: Development of the Spanish-language diabetes knowledge questionnaire. Diabetes Care. 2001;24(1):16-21. https://pubmed.ncbi.nlm.nih.gov/11194219. https://doi.org/10.2337/diacare.24.1.16.
Bukhsh A, Lee SWH, Pusparajah P, Khan AH, Khan TM. Psychometric properties of the Urdu version of Diabetes Knowledge Questionnaire. Front Public Health. 2017;5:139. https://pubmed.ncbi.nlm.nih.gov/28702453. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5484766. https://doi.org/10.3389/fpubh.2017.00139.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25(24):3186-91. https://pubmed.ncbi.nlm.nih.gov/11124735. https://doi.org/10.1097/00007632-200012150-00014.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB.. Recommendations for the cross-cultural adaptation of the DASH & QuickDASH outcome measures. Institute for Work & Health, 2007. https://dash.iwh.on.ca/sites/dash/files/downloads/cross_cultural_adaptation_2007.pdf
Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34-42. https://pubmed.ncbi.nlm.nih.gov/17161752. https://doi.org/10.1016/j.jclinepi.2006.03.012.
Bowling A. Research methods in health: Investigating health and health services. 4th ed. Berkshire: McGraw Hill Education Open University Press, 2014. https://doi.org/10.1027//0269-8803.14.2.126
Altman DG. Practical statistics for medical research. 1st ed. New York: CRC Press, 1990.
Machado RDS, Fernandes ADdBF, de Oliveira ALCB, Soares LS, Gouveia MTdO, da Silva GRF. Cross-cultural adaptation methods of instruments in the nursing area. Rev Gaucha Enferm. 2018;39:e20170164. https://pubmed.ncbi.nlm.nih.gov/29995073. https://doi.org/10.1590/1983-1447.2018.2017-0164.
Norozi E, Miri MR, Soltani R, Eslami AA, Harivandi AR, Dastjerdi R. Cultural adaptation and psychometric properties of the Persian version of the circumstances, motivation, and readiness scale. Int J High Risk Behav Addict. 2016;5(2):e23242. https://doi.org/10.5812/ijhrba.23242.
Kalantari R, Farahani AZ, Garosi E, Badeli H, Jamali J. Translation and psychometric properties of the Persian version of Oxford non-technical skills 2 system: Assessment of surgical teams' non-technical skills in orthopedic surgery wards. Arch Bone Jt Surg. 2019;7(2):173-81. https://pubmed.ncbi.nlm.nih.gov/31211196. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6510912.
de Raaij EJ, Schröder C, Maissan FJ, Pool JJ, Wittink H. Cross-cultural adaptation and measurement properties of the Brief Illness Perception Questionnaire-Dutch language version. Man Ther. 2012;17(4):330-5. https://pubmed.ncbi.nlm.nih.gov/22483222. https://doi.org/10.1016/j.math.2012.03.001.
Ebrahimzadeh MH, Birjandinejad A, Kachooei AR. Cross-cultural adaptation, validation, and reliability of the Michigan Hand Outcomes Questionnaire among Persian population. Hand Surg. 2015;20(1):25-31. https://pubmed.ncbi.nlm.nih.gov/25609271. https://doi.org/10.1142/S0218810415500033.
Published
How to Cite
Issue
Section
License
Journal of the ASEAN Federation of Endocrine Societies is licensed under a Creative Commons Attribution-NonCommercial 4.0 International. (full license at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.
















