Validation of Genome-Wide Association Studies (GWAS)-Identified Type 2 Diabetes Mellitus Risk Variants in Pakistani Pashtun Population
DOI:
https://doi.org/10.15605/jafes.037.S5Keywords:
Type 2 Diabetes Mellitus, European GWAS, SNPs validation, replication study, Pashtun populationAbstract
Objective. Recent GWAS largely conducted in European populations have successfully identified multiple genetic risk variants associated with Type 2 Diabetes Mellitus (T2DM). However, the effects conferred by these variants in the Pakistani population have not yet been fully elucidated. The objective of this study was to examine European GWAS- identified T2DM risk variants in the Pakistani Pashtun population to better understand the shared genetic basis of T2DM in the European and Pakistani cohorts.
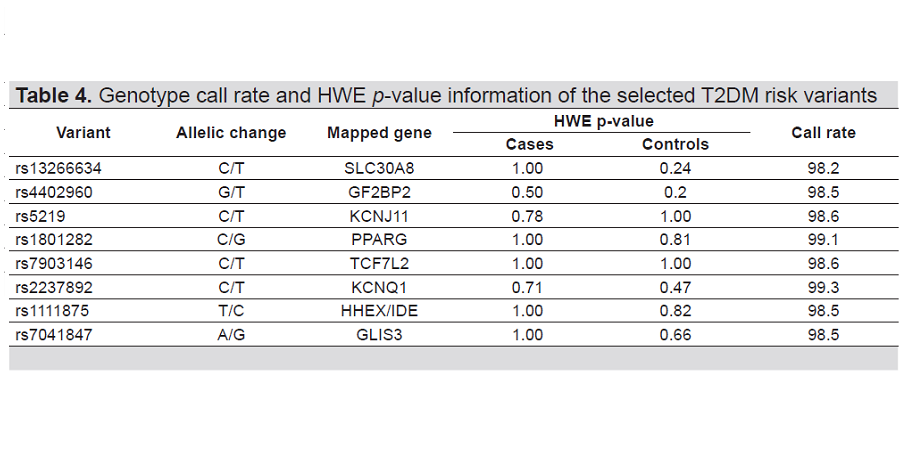
Methodology. A total of 100 T2DM patients and 100 healthy volunteers of Pashtun ethnicity were enrolled in this study. Both groups were genotyped for 8 selected single nucleotide polymorphisms (SNPs) using the Sequenom MassARRAY® platform. The association between selected SNPs and T2DM was determined by using appropriate statistical tests.
Results. Of the 8 studied SNPs, 5 SNPs, SLC30A8/ rs13266634 (p=0.031, OR=2.13), IGF2BP2/ rs4402960 (p=0.001, OR=3.01), KCNJ11/ rs5219 (p=0.042, OR=1.78), PPARG/ rs1801282 (p=0.042, OR=2.81) and TCF7L2/ rs7903146 (p=0.00006, 3.41) had a significant association with T2DM. SNP GLIS3/ rs7041847 (p=0.051, OR=2.01) showed no sufficient evidence of association. SNPs KCNQ1/ rs2237892 (p=0.140, OR=1.61) and HHEX/IDE/ s1111875 (p=0.112, OR=1.31) showed opposite allelic effects and were not validated for T2DM risk in the study population. Among the studied SNPs, TCF7L2/ rs7903146 showed the most significant association.
Conclusion. Our study finding indicates that selected genome-wide significant T2DM risk variants previously identified
in European descent also increase the risk of developing T2DM in the Pakistani Pashtun population.
Downloads
References
Colagiuri S. Definition and Classification of Diabetes and Prediabetes and Emerging Data on Phenotypes. Endocrinol Metab Clin North Am. 2021;50(3):319-36. https://pubmed.ncbi.nlm.nih.gov/34399948. https://doi.org/10.1016/j.ecl.2021.06.004.
Sun H, Saeedi P, Karuranga S, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2021:109119. https://pubmed.ncbi.nlm.nih.gov/34879977. https://doi.org/10.1016/j.diabres.2021.109119.
Association AD. 3. Prevention or delay of type 2 diabetes: Standards of Medical Care in Diabetes—2021. Diabetes Care. 2021;44(Supplement 1): S34-S9. https://pubmed.ncbi.nlm.nih.gov/33298414. https://doi.org/10.2337/dc21-S003.
Himanshu D, Ali W, Wamique M. Type 2 diabetes mellitus: Pathogenesis and genetic diagnosis. J Diabetes Metab Disord. 2020:1-8. https://pubmed.ncbi.nlm.nih.gov/33520871. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7843813. https://doi.org/10.1007/s40200-020-00641-x.
Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet. 2021. https://pubmed.ncbi.nlm.nih.gov/34600604 .https://doi.org/10.1016/S0140-6736(21)01919-X.
Li X, Zhou T, Ma H, Liang Z, Fonseca VA, Qi L. Replacement of sedentary behavior by various daily-life physical activities and structured exercises: Genetic risk and incident type 2 diabetes. Diabetes Care. 2021;44(10):2403-10. https://pubmed.ncbi.nlm.nih.gov/34183430. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8929188. https://doi.org/10.2337/dc21-0455.
Beulens JW, Pinho MG, Abreu TC, et al. Environmental risk factors of type 2 diabetes—An exposome approach. Diabetologia. 2021:1-12. https://pubmed.ncbi.nlm.nih.gov/34792619. https://doi.org/10.1007/s00125-021-05618-w.
Mambiya M, Shang M, Wang Y, et al. The play of genes and non-genetic factors on type 2 diabetes. Front. Public Health. 2019;7:349. https://pubmed.ncbi.nlm.nih.gov/31803711. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6877736. https://dx.doi.org/10.3389%2Ffpubh.2019.00349.
Lin X, Xu Y, Pan X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci Rep. 2020;10(1):1-11. https://pubmed.ncbi.nlm.nih.gov/32901098. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7478957. https://doi.org/10.1038/s41598-020-71908-9.
Cuschieri S. Type 2 diabetes–An unresolved disease across centuries contributing to a public health emergency. Diabetes Metab Syndr. 2019;13(1):450-3. https://pubmed.ncbi.nlm.nih.gov/30641742. https://doi.org/10.1016/j.dsx.2018.11.010.
Bommer C, Sagalova V, Heesemann E, et al. Global economic burden of diabetes in adults: Projections from 2015 to 2030. Diabetes Care. 2018;41(5):963-70. https://pubmed.ncbi.nlm.nih.gov/29475843. https://doi.org/10.2337/dc17-1962.
International Diabetes Federation. IDF Diabetes Atlas, 10th edn. Brussels, Belgium: 2021. Available at: https://www.diabetesatlas.org.
Flood D, Seiglie JA, Dunn M, et al. The state of diabetes treatment coverage in 55 low-income and middle-income countries: A cross-sectional study of nationally representative, individual-level data in 680 102 adults. Lancet Healthy Longev. 2021;2(6):e340-e51. https://pubmed.ncbi.nlm.nih.gov/35211689. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8865379. https://doi.org/10.1016/S2666-7568(21)00089-1.
Banerjee AT, Shah B. One Size Does Not Fit All: Diabetes Prevalence Among Immigrants of the South Asian Diaspora. J Immigr Minor Health. 2020:1-6. https://pubmed.ncbi.nlm.nih.gov/32990901. https://doi.org/10.1007/s10903-020-01093-4.
Narayan KV, Kondal D, Daya N, et al. Incidence and pathophysiology of diabetes in South Asian adults living in India and Pakistan compared with US blacks and whites. BMJ Open Diabetes Res Care.. 2021;9(1):e001927. https://pubmed.ncbi.nlm.nih.gov/33771764. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8006839. http://dx.doi.org/10.1136/bmjdrc-2020-001927.
Akhtar S, Nasir JA, Abbas T, Sarwar A. Diabetes in Pakistan: A systematic review and meta-analysis. Pak J Med Sci. 2019;35(4):1173. https://pubmed.ncbi.nlm.nih.gov/31372163. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6659044. https://doi.org/10.12669/pjms.35.4.194.
Basit A, Fawwad A, Qureshi H, Shera A. Prevalence of diabetes, pre-diabetes and associated risk factors: Second National Diabetes Survey of Pakistan (NDSP), 2016–2017. BMJ Open. 2018;8(8):e020961. https://pubmed.ncbi.nlm.nih.gov/30082350. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6078264. http://dx.doi.org/10.1136/bmjopen-2017-020961corr1.
Almgren P, Lehtovirta M, Isomaa B, et al. Heritability and familiality of type 2 diabetes and related quantitative traits in the Botnia Study. Diabetologia. 2011;54(11):2811-9. https://pubmed.ncbi.nlm.nih.gov/21826484 .https://doi.org/10.1007/s00125-011-2267-5.
Meigs JB, Cupples LA, Wilson P. Parental transmission of type 2 diabetes: The Framingham Offspring Study. Diabetes. 2000;49(12):2201-7. https://pubmed.ncbi.nlm.nih.gov/11118026. https://doi.org/10.2337/diabetes.49.12.2201.
Jackson M, Marks L, May GH, Wilson JB. The genetic basis of disease. Essays Biochem. 2018;62(5):643-723. https://pubmed.ncbi.nlm.nih.gov/30509934. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6279436. https://dx.doi.org/10.1042%2FEBC20170053.
Fuchsberger C, Flannick J, Teslovich TM, et al. The genetic architecture of type 2 diabetes. Nature. 2016;536(7614):41-7. https://pubmed.ncbi.nlm.nih.gov/27398621. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5034897. https://doi.org/10.1038/nature18642.
Krentz NA, Gloyn AL. Insights into pancreatic islet cell dysfunction from type 2 diabetes mellitus genetics. Nat Rev Endocrinol. 2020; 16(4):202-12. https://pubmed.ncbi.nlm.nih.gov/32099086. https://doi.org/10.1038/s41574-020-0325-0.
Martin AR, Kanai M, Kamatani Y, Okada Y, Neale BM, Daly MJ. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat Genet. 2019;51(4):584-91. https://pubmed.ncbi.nlm.nih.gov/30926966. https://doi.org/10.1038/s41588-019-0379-x.
Batool H, Mushtaq N, Batool S, et al. Identification of the potential type 2 diabetes susceptibility genetic elements in South Asian populations. Meta Gene. 2020 1; 26:100771. http://dx.doi.org/10.1016/j.mgene.2020.100771.
Akhtar S, Khan Z, Rafiq M, Khan A. Prevalence of type II diabetes in District Dir Lower in Pakistan. Pak J Med Sci. 2016; 32(3):622. https://pubmed.ncbi.nlm.nih.gov/27375702. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4928411. https://dx.doi.org/10.12669%2Fpjms.323.9795.
Riaz M, Tiller J, Ajmal M, Azam M, Qamar R, Lacaze P. Implementation of public health genomics in Pakistan. European Journal of Human Genetics. 2019; 27(10):1485-92. https://pubmed.ncbi.nlm.nih.gov/31101884. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6777461. https://doi.org/10.1038/s41431-019-0428-z
Shabana SU, Li KW, Acharya J, Cooper JA, Hasnain S, Humphries SE. Effect of six type II diabetes susceptibility loci and an FTO variant on obesity in Pakistani subjects. Eur J Hum Genet. 2016; 24(6):903. https://pubmed.ncbi.nlm.nih.gov/26395551. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4867451.https://doi.org/10.1038/ejhg.2015.212.
Butt H, Hasnain S. The C1431T polymorphism of peroxisome proliferator-activated receptor γ (PPARγ) is associated with low risk of diabetes in a Pakistani cohort. Diabetol Metab Syndr. 2016 Dec;8(1):1-6. https://pubmed.ncbi.nlm.nih.gov/27625707. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5020519.https://doi.org/10.1186/s13098-016-0183-z.
Welter D, MacArthur J, Morales J, et al. The NHGRI GWAS Catalog, a curated resource of SNP-trait associations. Nucleic Acids Res. 2014 1;42(D1):D1001-6. https://pubmed.ncbi.nlm.nih.gov/24316577. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3965119. https://doi.org/10.1093/nar/gkt1229.
MacArthur J, Bowler E, Cerezo M, et al. The new NHGRI-EBI Catalog of published genome-wide association studies (GWAS Catalog). Nucleic Acids Res. 2017 4;45(D1):D896-901. https://pubmed.ncbi.nlm.nih.gov/27899670. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5210590. https://doi.org/10.1093/nar/gkw1133.
Gabriel S, Ziaugra L, Tabbaa D. SNP genotyping using the Sequenom MassARRAY iPLEX platform. Curr Protoc Hum Genet. 2009; 60(1):2-12. https://pubmed.ncbi.nlm.nih.gov/19170031. https://doi.org/10.1002/0471142905.hg0212s60.
Lee WC. Optimal trend tests for genetic association studies of heterogeneous diseases. Sci Rep. 2016; 6(1):1-7. https://pubmed.ncbi.nlm.nih.gov/27278756. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4899796. https://doi.org/10.1038/srep27821.
Jan A, Saeed M, Afridi MH, et al. Association of HLA-B Gene Polymorphisms with Type 2 Diabetes in Pashtun Ethnic Population of Khyber Pakhtunkhwa, Pakistan. J Diabetes Res. 2021; 16: 2021. https://pubmed.ncbi.nlm.nih.gov/34258292. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8254654. https://doi.org/10.1155/2021/6669731.
Zia A, Wang X, Bhatti A, et al. A replication study of 49 Type 2 diabetes risk variants in a Punjabi Pakistani population. Diabet Med. 2016; 33(8):1112-7. https://pubmed.ncbi.nlm.nih.gov/26499911. https://doi.org/10.1111/dme.13012.
Rees SD, Hydrie MZ, Shera AS, et al. Replication of 13 genome-wide association (GWA)-validated risk variants for type 2 diabetes in Pakistani populations. Diabetologia. 2011; 54(6):1368-74. https://pubmed.ncbi.nlm.nih.gov/21350842. https://doi.org/10.1007/s00125-011-2063-2.
Sabiha B, Bhatti A, Fan KH, et al. Assessment of genetic risk of type 2 diabetes among Pakistanis based on GWAS-implicated loci. Gene. 2021; 30;783:145563. https://pubmed.ncbi.nlm.nih.gov/33705809. https://doi.org/10.1016/j.gene.2021.145563.
Jaacks LM, Siegel KR, Gujral UP, Narayan KV. Type 2 diabetes: A 21st century epidemic. Best Pract Res Clin Endocrinol Metab. 2016; 30(3):331-43. https://pubmed.ncbi.nlm.nih.gov/27432069. https://doi.org/10.1016/j.beem.2016.05.003.
Kido Y. Gene–environment interaction in type 2 diabetes. Diabetol Int. 2017; 8(1):7-13. https://pubmed.ncbi.nlm.nih.gov/30603301. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6224936. https://doi.org/10.1007/s13340-016-0299-2.
Peterson RE, Kuchenbaecker K, Walters RK, et al. Genome-wide association studies in ancestrally diverse populations: Opportunities, methods, pitfalls, and recommendations. Cell. 2019; 179(3):589-603. https://pubmed.ncbi.nlm.nih.gov/31607513. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6939869. https://doi.org/10.1016/j.cell.2019.08.051.
Basit A, Fawwad A, Siddiqui SA, Baqa K. Current management strategies to target the increasing incidence of diabetes within Pakistan. Diabetes Metab Syndr Obes. 2019; 12:85. https://pubmed.ncbi.nlm.nih.gov/30643443. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6314051 https://doi.org/10.2147/DMSO.S141356.
Vujkovic M, Keaton JM, Lynch JA, et al. Discovery of 318 new risk loci for type 2 diabetes and related vascular outcomes among 1.4 million participants in a multi-ancestry meta-analysis. Nat Genet. 2020; 52(7):680-91. https://pubmed.ncbi.nlm.nih.gov/32541925. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7343592. https://doi.org/10.1038/s41588-020-0637-y.
Mahajan A, Go MJ, Zhang W, et al. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat Genet. 2014; 46(3):234-44. https://pubmed.ncbi.nlm.nih.gov/24509480. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3969612. https://doi.org/10.1038/ng.2897.
Scott RA, Scott LJ, Mägi R, et al. An expanded genome-wide association study of type 2 diabetes in Europeans. Diabetes. 2017; 66(11):2888-902. https://pubmed.ncbi.nlm.nih.gov/28566273. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5652602. https://doi.org/10.2337/db16-1253.
Scott LJ, Mohlke KL, Bonnycastle LL, et al. A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science. 2007; 316(5829):1341-5. https://pubmed.ncbi.nlm.nih.gov/17463248. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3214617. https://doi.org/10.1126/science.1142382.
Yasuda K, Miyake K, Horikawa Y, et al. Variants in KCNQ1 are associated with susceptibility to type 2 diabetes mellitus. Nat Genet. 2008; 40(9):1092-7. https://pubmed.ncbi.nlm.nih.gov/18711367. https://doi.org/10.1038/ng.207.
Li YY, Wang XM, Lu XZ. KCNQ 1 rs2237892 C→ T gene polymorphism and type 2 diabetes mellitus in the Asian population: A metaanalysis of 15,736 patients. J Cell Mol Med. 2014; 18(2):274-82. https://pubmed.ncbi.nlm.nih.gov/24373634. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3930414. https://doi.org/10.1111/jcmm.12185.
Cai Y, Yi J, Ma Y, Fu D. Meta-analysis of the effect of HHEX gene polymorphism on the risk of type 2 diabetes. Mutagenesis. 2011; 26(2):309-14. https://pubmed.ncbi.nlm.nih.gov/21059810. https://doi.org/10.1093/mutage/geq095.
Li C, Shen K, Yang M, et al. Association between single nucleotide polymorphisms in CDKAL1 and HHEX and type 2 diabetes in Chinese population. Diabetes Metab Syndr Obes. 2020; 13:5113. https://pubmed.ncbi.nlm.nih.gov/33447064. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7801916. https://doi.org/10.2147/DMSO.S288587.
Plengvidhya N, Chanprasert C, Chongjaroen N, Yenchitsomanus PT, Homsanit M, Tangjittipokin W. Impact of KCNQ1, CDKN2A/2B, CDKAL1, HHEX, MTNR1B, SLC30A8, TCF7L2, and UBE2E2 on risk of developing type 2 diabetes in Thai population. BMC Med Genet. 2018; 19(1):1-9. https://pubmed.ncbi.nlm.nih.gov/29871606. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5989367. https://doi.org/10.1186/s12881-018-0614-9.
Ding W, Xu L, Zhang L, et al. Meta-analysis of association between TCF7L2 polymorphism rs7903146 and type 2 diabetes mellitus. BMC Med Genet. 2018; 19(1):1-2. https://pubmed.ncbi.nlm.nih.gov/29514658. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5842570. https://doi.org/10.1186/s12881-018-0553-5.
Lyssenko V, Lupi R, Marchetti P, et al. Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest. 2007; 117(8):2155-63. https://pubmed.ncbi.nlm.nih.gov/17671651. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1934596. https://doi.org/10.1172/jci30706.
Jan A, Jan H, Ullah Z. Transcription factor 7-like 2 (TCF7L2): A culprit gene in Type 2 Diabetes Mellitus. Diabetes mellitus. 2021; 24(4):371-6. https://doi.org/10.14341/DM12313.
Ip W, Chiang YT, Jin T. The involvement of the wnt signaling pathway and TCF7L2 in diabetes mellitus: The current understanding, dispute, and perspective. Cell Biosci. 2012; 2(1):1-2. https://pubmed.ncbi.nlm.nih.gov/22892353. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3468386. https://doi.org/10.1186/2045-3701-2-28.
Takeuchi F, Serizawa M, Yamamoto K, et al. Confirmation of multiple risk Loci and genetic impacts by a genome-wide association study of type 2 diabetes in the Japanese population. Diabetes. 2009; 58(7):1690-9. https://pubmed.ncbi.nlm.nih.gov/19401414. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699880. https://doi.org/10.2337/db08-1494.
Rao P, Wang H, Fang H, et al. Association between IGF2BP2 polymorphisms and type 2 diabetes mellitus: A case-control study and meta-analysis. Int J Environ Res Public Health. 2016; 13(6):574. https://pubmed.ncbi.nlm.nih.gov/27294943. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4924031. https://dx.doi.org/10.3390%2Fijerph13060574.
Chistiakov DA, Nikitin AG, Smetanina SA, et al. The rs11705701 G> A polymorphism of IGF2BP2 is associated with IGF2BP2 mRNA and protein levels in the visceral adipose tissue-a link to type 2 diabetes susceptibility. Rev Diabet Stud. RDS. 2012; 9(2-3):112. https://pubmed.ncbi.nlm.nih.gov/23403707. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3700024. https://doi.org/10.1900/rds.2012.9.112.
Regine I, Husain RS, Aswathi RP, Reddy DR, Ahmed SS, Ramakrishnan V. Association between PPARγ rs1801282 polymorphism with diabetic nephropathy and type-2 diabetes mellitus susceptibility in south India and a meta-analysis. Nefrología (English Edition). 2020; 40(3):287-98. https://pubmed.ncbi.nlm.nih.gov/32417009. https://doi.org/10.1016/j.nefro.2020.01.005.
Bakhashab S, Filimban N, Altall RM, et al. The effect sizes of PPARγ rs1801282, FTO rs9939609, and MC4R rs2229616 variants on type 2 diabetes mellitus risk among the western Saudi population: A cross-sectional prospective study. Genes. 2020; 11(1):98. https://pubmed.ncbi.nlm.nih.gov/31947684. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7017045. https://doi.org/10.3390/genes11010098.
Yen CJ, Beamer BA, Negri C, et al. Molecular scanning of the human peroxisome proliferator-activated receptor γ (hPPARγ) gene in diabetic Caucasians: Identification of a Pro12Ala PPARγ2 missense mutation. Biochem Biophys Res Commun. 1997; 241(2):270-4. https://pubmed.ncbi.nlm.nih.gov/9425261. https://doi.org/10.1006/bbrc.1997.7798.
Radha V, Mohan V. Genetic predisposition to type 2 diabetes among Asian Indians. Indian J Med Res. 2007; 125(3):259-74. https://pubmed.ncbi.nlm.nih.gov/17496355. https://pubmed.ncbi.nlm.nih.gov/17496355/.
Majid M, Masood A, Kadla SA, Hameed I, Ganai BA. Association of Pro12Ala polymorphism of peroxisome proliferator-activated receptor gamma 2 (PPARγ2) gene with type 2 diabetes mellitus in ethnic Kashmiri population. Biochem Genet. 2017; 55(1):10-21. https://pubmed.ncbi.nlm.nih.gov/27567620. https://doi.org/10.1007/s10528-016-9765-6.
Vergotine Z, Yako YY, Kengne AP, Erasmus RT, Matsha TE. Proliferator-activated receptor gamma Pro12Ala interacts with the insulin receptor substrate 1 Gly972Arg and increases the risk of insulin resistance and diabetes in the mixed ancestry population from South Africa. BMC Genet. 2014; 15(1):1-8. https://pubmed.ncbi.nlm.nih.gov/24447396. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3900266. https://doi.org/10.1186/1471-2156-15-10.
Imamura M, Takahashi A, Yamauchi T, et al. Genome-wide association studies in the Japanese population identify seven novel loci for type 2 diabetes. Nat Commun. 2016; 7(1):1-2. https://pubmed.ncbi.nlm.nih.gov/26818947. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4738362. https://doi.org/10.1038/ncomms10531.
Wang DD, Chen X, Yang Y, Liu CX. Association of Kir6. 2 gene rs5219 variation with type 2 diabetes: A meta-analysis of 21,464 individuals. Prim Care Diabetes. 2018; 12(4):345-53. https://pubmed.ncbi.nlm.nih.gov/29685723. https://doi.org/10.1016/j.pcd.2018.03.004.
Salem SD, Saif-Ali R, Ismail IS, Al-Hamodi Z, Muniandy S. Contribution of SLC30A8 variants to the risk of type 2 diabetes in a multi-ethnic population: A case-control study. BMC Endocr Disord. 2014; 14(1):1-7. https://pubmed.ncbi.nlm.nih.gov/24393180. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3893602. https://doi.org/10.1186/1472-6823-14-2.
Dong F, Zhang BH, Zheng SL, et al. Association between SLC30A8 rs13266634 polymorphism and risk of T2DM and IGR in Chinese population: A systematic review and meta-analysis. Front Endocrinol (Lausanne). 2018; 9:564. https://pubmed.ncbi.nlm.nih.gov/30319545. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6167413. https://dx.doi.org/10.3389%2Ffendo.2018.00564.
Haghvirdizadeh P, Mohamed Z, Abdullah NA, Haghvirdizadeh P, Haerian MS, Haerian BS. KCNJ11: Genetic polymorphisms and risk of diabetes mellitus. J Diabetes Res. 2015; 2015.1-10. https://pubmed.ncbi.nlm.nih.gov/26448950. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4584059. https://doi.org/10.1155/2015/908152.
Riedel MJ, Steckley DC, Light PE. Current status of the E23K Kir6. 2 polymorphism: Implications for type-2 diabetes. Hum Genet. 2005; 116(3):133-45. https://pubmed.ncbi.nlm.nih.gov/15565284. https://doi.org/10.1007/s00439-004-1216-5.
Liu C, Li H, Qi L, Loos RJ, Qi Q, Lu L, Gan W, Lin X. Variants in GLIS3 and CRY2 are associated with type 2 diabetes and impaired fasting glucose in Chinese Hans. PLoS One. 2011; 6(6):e21464. https://pubmed.ncbi.nlm.nih.gov/21747906. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3126830. https://doi.org/10.1371/journal.pone.0021464.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Asif Jan, Zakiullah, Fazli Khuda, Rani Akbar

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Journal of the ASEAN Federation of Endocrine Societies is licensed under a Creative Commons Attribution-NonCommercial 4.0 International. (full license at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.
















